
Sacral Insufficiency Fracture: What It Is, Why It Happens, and Why It’s Often Missed
Sacral Insufficiency Fracture is a stress fracture that occurs when weakened bone can no longer tolerate normal everyday loading.
Sacral insufficiency fracture is a condition that often causes confusion — and frustration — because it doesn’t behave like most people expect a fracture to behave.
There’s usually no fall, no accident, and no dramatic injury. Instead, pain develops gradually, often presenting as lower back, buttock, hip or pelvic pain that simply doesn’t settle. Because of this, sacral insufficiency fractures are frequently mistaken for arthritis, degenerative spine problems, or “just another back issue”.
Understanding what this type of fracture really is — and why it’s commonly missed — is key to getting the right diagnosis and avoiding unnecessary delays in recovery.
Get WISE - Get WELL - Get ON
What Is A Sacral Insufficiency Fracture?
The sacrum is the triangular bone at the base of your spine that connects the spine to the pelvis. It plays a crucial role in transferring load from your upper body into your legs when you stand and walk.
A sacral insufficiency fracture is a type of stress (or fragility) fracture. It occurs when normal, everyday forces — such as standing, walking, or rising from a chair — are applied to bone that has become weakened.
This is very different from a fracture caused by trauma. In this case, the problem isn’t excessive force — it’s reduced bone strength.
Importantly, this means a sacral insufficiency fracture can occur without any clear injury.
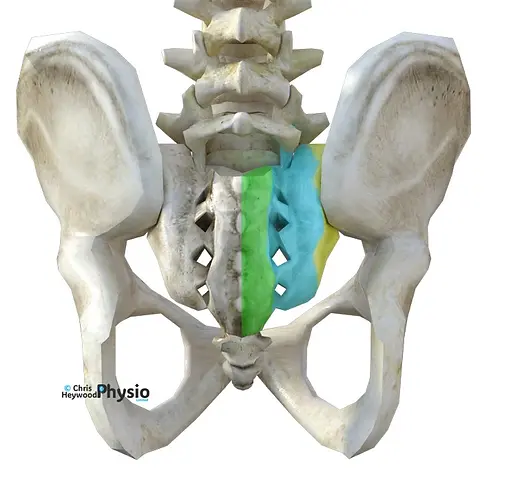
Denis et al (3), divided the sacrum up into three separate zones:
1) Outer Sacrum - Zone 1 (Yellow)
2) Mid Sacrum - Zone 2 (Blue)
3) Inner Sacrum - Zone 3 (Green
Why Do Sacral Insufficiency Fractures Happen?
Most sacral insufficiency fractures develop because the bone is no longer able to tolerate normal loading.
The most common contributing factors include:
-
Reduced bone density, such as osteoporosis or osteopenia
-
Increasing age, particularly in post-menopausal women
-
Long-term use of medications that affect bone strength (for example corticosteroids)
-
Medical conditions that interfere with bone metabolism
-
Previous pelvic radiotherapy, which can weaken bone over time
Elderly Women With Osteoporosis :- Osteoporosis weakens bones, making them more susceptible to fractures from minor falls or injuries. Up to half of women and 20% of men over 50 who suffer fractures do so due to reduced bone strength. For more info
Previous Pelvic Radiation :- Radiation therapy, often used in cancer treatment, can degrade bone quality in the treated area. This risk is especially notable for cancers of the bladder, rectum, prostate, cervix, womb, and vagina. For more info
Multiple Myeloma :- Multiple Myeloma is a type of cancer that affects the white blood cells, more specifically a plasma cell, that is found inside our bone marrow. White blood cells normally help to neutralise pathogens such as bacteria and viruses by producing antibodies. Abnormal plasma cells can go on to form masses within bone, such as the pelvis altering the strength and quality and subsequent risk of fracture. For more info
Paget's Disease :- Paget's Disease is a condition that effects the normal ''repair and renewal' process that we see in healthy bone metabolism. Bones are under a constant cycle whereby old bone is broken down, removed, and replaced by new bone. In Paget's disease the balance of this process is altered, leading to an increased volume of overall bone turnover that can make new bone weak and and brittle. For more info
Renal Osteodystrophy :- Renal Osteodystrophy is a type of bone disease that is caused by having a long term, elevated level of Parathyroid Hormone in your blood stream. This can cause an increased level of calcium to be removed from your bones making the natural reparative cycle of bone increasingly inefficient. It is normally associate with chronic kidney disease. For more info
Steroid Induced Osteopenia :- Steroid Induced Osteopenia refers to the thinning of the bones that we can occur in people who are on long term steroids. This can include inhalers, prescribed for some breathing complaints, and tablets such as Prednisolone, with the general definition of long-term being everyday for more than 3 months. Steroid creams may carry less of a risk. For more info
Hyperparathyroidism :- Parathyroid Hormone has a direct effect on the levels of calcium, phosphorus and vitamin D in our blood and bones. It is produced by 4 Parathyroid Glands that are found behind the Thyroid Gland in the neck. HYPER-Parathyroidism refers to when elevated levels of the hormone are produced which can in turn lead to Chronic Kidney Disease and Renal Osteodystrophy, as above. For more info
Rheumatoid Arthritis :- Rheumatoid Arthritis (RA) is an autoimmune disorder that commonly causes joint inflammation. The process that underlies the condition can also affect the bone matrix - the architectural makeup of the bone itself, which can lead to bone weakness and poor. For more info
Less commonly, sacral insufficiency fractures can occur in younger people, usually where bone health has been affected or loading demands have changed significantly.
The important point is this:
A sacral insufficiency fracture can occur without any obvious injury.
How Does A Sacral Insufficiency Fracture Feel?
One of the reasons this condition is often missed is that the symptoms are non-specific and can mimic other, more common problems.
People commonly describe:
-
Pain in the lower back, buttock, pelvis or hip region
-
Pain that worsens with standing or walking and eases with rest
-
Reduced walking tolerance or difficulty weight-bearing
-
Pain when moving from sitting to standing
-
Symptoms that feel similar to sciatica, hip arthritis, or sacroiliac joint pain
The pain often builds gradually and doesn’t feel like a sudden “fracture”, which is why it’s frequently attributed to something else.
Why Are Sacral Insufficiency Fractures So Often Missed?
There are three main reasons:
First, the symptoms overlap with common conditions such as degenerative disc disease, hip arthritis, or general low back pain.
Second, standard X-rays often fail to show the fracture, particularly in the early stages. The sacrum is a complex structure, and subtle fractures can be difficult to visualise.
Third, the absence of trauma can lead both patients and clinicians away from considering a fracture in the first place.
As a result, diagnosis is often delayed — sometimes for weeks or months.
How Are Sacral Insufficiency Fractures Diagnosed?
When a sacral insufficiency fracture is suspected, more sensitive imaging is usually required.
This typically involves:
-
MRI scanning, which can detect bone stress and inflammation even when a clear fracture line isn’t visible
-
CT scanning, which can help define the fracture pattern more clearly
Imaging should always be interpreted alongside a full clinical assessment, including symptoms, risk factors, and overall bone health.
What Is The Usual Treatment For SIF's?
Most sacral insufficiency fractures are managed without surgery.
Treatment generally focuses on three key areas:
Protecting the fracture without complete rest
Prolonged bed rest is rarely helpful and can actually slow recovery by increasing muscle weakness and further bone loss. Instead, management usually involves relative rest — reducing painful activities while maintaining safe, gentle movement.
Managing pain and restoring function
Pain relief may be needed initially. Physiotherapy can then help guide a gradual return to movement, walking tolerance, strength, and confidence — without overloading the healing bone.
Addressing underlying bone health
Because sacral insufficiency fractures are often linked to reduced bone strength, it’s important that bone health is properly assessed and managed. This may include bone density scanning, medication, and addressing nutritional or hormonal factors where appropriate.
What About Procedures Like Sacroplasty?
In some cases — particularly where pain remains severe and disabling despite appropriate conservative care — a procedure called Sacroplasty may be considered.
Sacroplasty involves injecting bone cement into the fracture area to improve stability and reduce pain. While it can be helpful for selected individuals, it is generally reserved for situations where recovery has stalled and quality of life is significantly affected.
It is not a first-line treatment, and careful patient selection is essential.
Sacroplasty is a procedure where a special cement PMMA (Polymethyl Methacrylate) is injected under image guidance, into the sacral fracture site(s). It is a fairly new technique that has been derived from a more longstanding procedure called Kyphoplasty, which involves injecting the PMMA in to a vertebral body in the spine instead There are two main techniques: 1) The Posterior Approach 2) The Long-Axis Approach More recently there has been an introduction of a Sacral Kyphoplasty but this is significantly less common than the aforementioned techniques so will not be discussed further at present. As with many new medical procedures the problem of good, strong evidence is limited and only time will solve this however the research that has been undertaken to date is very positive on the whole. Akin to spinal disc prolapses, there is an acceptance that spontaneous recovery will, in most, occur naturally in 12 months (on average), so conservative management is championed by many. For those that don't heal however, are in too much pain, or where the conservative management (which is structured around significantly reduced mobility) is not ideal, Sacroplasty may be an option. Sacroplasty has very limited patient based education available which is why this initial page has been created. If you do want further reading however the two papers listed below offer excellent insight and can be accessed by Google with no fee or memberships required. They both use medical terminology which may be difficult for some to understand however as more information and pictures become available we will endeavour to feature this in an easy to understand format.
How Long Does Recovery Take?
Recovery times vary depending on:
-
the extent of the fracture
-
underlying bone health
-
overall fitness and mobility
-
how early the condition is identified
Many people improve gradually over weeks to months with appropriate management. Early recognition and correct diagnosis tend to lead to better outcomes.
When Should You Seek Further Medical Advice?
You should seek prompt medical review if you experience:
-
severe or worsening pain with weight-bearing
-
new difficulty walking
-
pain that does not improve with rest
-
symptoms alongside known osteoporosis or recent cancer treatment
Early investigation is important — not because this condition is dangerous, but because missing it delays recovery.
The Key Message
Sacral insufficiency fractures are uncommon, but important to recognise.
They:
-
often occur without trauma
-
are frequently mistaken for other causes of back or hip pain
-
usually respond well to appropriate, timely management
Most importantly, they are treatable, and recovery is very possible when the right diagnosis is made.
The following paper's were very helpful in the construction of this page so are acknowledged:
Lyders EM, Whitlow CT, Baker MD, Morris PP. Imaging and Treatment of Sacral Insufficiency Fractures. Am J Neuroradiol 2010;31:201-10 (excellent for reading around the subject and getting a global overview)
Health Net National Medical Policy: Percutaneous Sacroplasty. (Very good review paper of present research and outcomes)References:(1)
Lourie H. Spontaneous osteoporotic fracture of the sacrum: an unrecognised syndrome in the elderly. JAMA 1982;248:715-17(2)
Lyders EM, Whitlow CT, Baker MD, Morris PP. Imaging and Treatment of Sacral Insufficiency Fractures. Am J Neuroradiol 2010;31:201-10(3)
Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Clin Orthop Relat Res 1988;227:67-81(4)
De Smet AA, Neff JR. Pubic and sacral insufficiency fractures: clinical course and radiologic findings. AJR Am J Roentgenol 1985; 145:601-06
Frequently Asked Questions about Sacral Insufficiency Fractures
1) What is a sacral insufficiency fracture?
A sacral insufficiency fracture is a type of stress fracture that occurs in the sacrum, the bone at the base of the spine. Unlike fractures caused by a fall or accident, it happens when normal everyday forces act on bone that has become weakened, most commonly due to reduced bone density.
2) Can you get a sacral insufficiency fracture without falling?
Yes. In fact, many sacral insufficiency fractures occur without any obvious injury. Simple activities such as standing, walking, or getting up from a chair can be enough to cause a fracture when the bone is already weakened.
3) What does a sacral insufficiency fracture feel like?
Symptoms are often vague and non-specific. People commonly describe:
-
lower back, buttock or pelvic pain
-
pain that worsens with standing or walking
-
difficulty weight-bearing
-
pain when moving from sitting to standing
Because the pain doesn’t always feel sharp or sudden, it’s often mistaken for arthritis or general back pain.
4) Who is most at risk of sacral insufficiency fractures?
Sacral insufficiency fractures are more common in:
-
people with osteoporosis or low bone density
-
post-menopausal women
-
older adults
-
people who have had pelvic radiotherapy
-
those on long-term steroid medication
They are less common in younger people, but can still occur if bone health is compromised.
5) Why are sacral insufficiency fractures often missed?
They’re often missed because:
-
symptoms mimic common back or hip conditions
-
X-rays frequently appear normal, especially early on
-
there is often no history of trauma
MRI or CT scans are usually needed to make the diagnosis.
5) How is a sacral insufficiency fracture diagnosed?
Diagnosis typically involves MRI scanning, which can detect bone stress and inflammation even when a fracture line isn’t visible. CT scans may also be used to define the fracture more clearly. Imaging is always interpreted alongside a full clinical assessment.
6) Do sacral insufficiency fractures heal on their own?
In many cases, yes. With appropriate management — including activity modification, pain control, and addressing underlying bone health — sacral insufficiency fractures often heal gradually over time. Recovery can take several weeks to months.
7) Is bed rest necessary for a sacral insufficiency fracture?
Complete bed rest is rarely recommended. Prolonged inactivity can worsen bone loss, muscle weakness, and overall recovery. Instead, most people benefit from relative rest, meaning painful activities are reduced while safe, gentle movement is encouraged.
8) What treatments are used for sacral insufficiency fractures?
Treatment usually focuses on:
-
managing pain
-
maintaining safe mobility
-
gradually restoring strength and function
-
improving bone health (e.g. osteoporosis management)
Physiotherapy often plays a role in guiding movement and rehabilitation once pain allows.
9) Will I need surgery or sacroplasty?
Most people do not need surgery. A procedure called sacroplasty may be considered in a small number of cases where pain remains severe and disabling despite conservative treatment. It’s generally reserved for carefully selected patients and is not first-line treatment.
Why You Should Choose Chris Heywood Physio
The most important thing when seeking help is finding a practitioner you trust—someone who is honest, responsible, and clear about your diagnosis, the treatment you really need, and whether any follow-up appointments are necessary.
I’m not here to poach you from another therapist, but if you’re looking for a new physiotherapist in Northamptonshire or simply want a second opinion, here’s why many people choose to work with me (read my reviews):
Over 25 Years of Experience & Proven Expertise
With 25+ years of hands-on physiotherapy experience, I’ve built a trusted reputation for clinical excellence and evidence-based care. My approach combines proven techniques with the latest research, so you can feel confident you’re in safe, skilled hands.
Longer Appointments for Better Results
No two people—or injuries—are the same. That’s why I offer 60-minute one-to-one sessions, giving us time to:
-
Thoroughly assess your condition
-
Provide focused, effective treatment
-
Explain what’s really going on in a clear, simple way
Your treatment plan is tailored specifically to you, aiming for long-term results, not just temporary relief.
Honest Advice & Support You Can Trust
I’ll always tell you what’s best for you—even if that means you need fewer sessions, not more. My goal is your recovery and wellbeing, not keeping you coming back unnecessarily. I have low overheads nowadays and I do not have pre-set management targets to maximise patient 'average session per condition' (yes it does happen commonly and I hate it with a passion - read my article here)
Helping You Take Control of Your Recovery
I believe the best outcomes happen when you understand your body. I’ll explain your condition clearly, give you practical tools for self-management, and step in with expert hands-on treatment when it’s genuinely needed.
Looking for a physiotherapist who values honesty, expertise, and your long-term health?
Book an appointment today and take the first step towards feeling better.
Contact Info
On a Monday and Tuesday I work as a advance musculoskeletal specialist in primary care but I can still be contacted for enquiries. You are welcome to call but it is often faster for me to reply via an email or watsapp message, simply as my phone will be on silent in clinic. Either way, I will reply as soon as possible, which in the week, is almost always on the same day at the latest.

Clinic Opening Hours
** Please note that online sessions and Aquatic sessions be arranged outside of normal clinical hours on request.**
Sat -Sun
Closed
0900 - 1430
Closed - FCP
Weds - Fri
Mon - Tues










